Gastroshiza might not be a term you’ve heard before, but for those affected by this rare condition, it represents a significant part of their lives. Imagine the struggle and challenges that come with having abdominal organs develop outside the body. This condition can evoke fear and uncertainty in families facing it. However, advances in medical science are shedding light on gastroshiza, providing hope through various treatment options.
Understanding gastroshiza is crucial for patients, caregivers, and even healthcare professionals. It’s essential to explore its causes, symptoms, and the latest approaches to treatment. Whether you’re seeking information for yourself or someone you care about, diving deep into this topic will empower you with knowledge that can make a difference. Let’s unravel the complexities of gastroshiza together!
What is Gastroshiza?
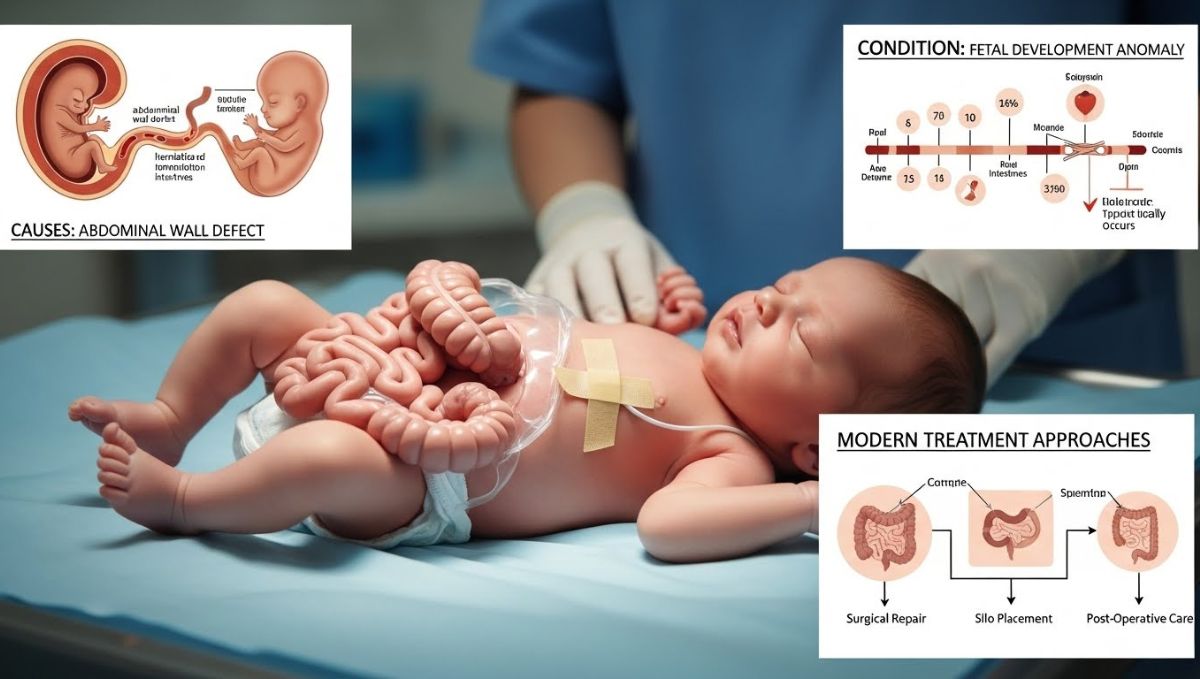
Gastroshiza is a congenital defect that occurs during fetal development. It results in the intestines and sometimes other abdominal organs being situated outside of the body, usually to the right side of the umbilical cord.
This condition arises when the abdominal wall does not close properly. As a result, various sections of the intestines are exposed to amniotic fluid rather than being protected within the abdomen.
Gastroshiza is distinct from similar conditions like omphalocele, where organs are covered by a membrane. In gastroshiza, there’s typically no such protective layer.
The exact prevalence remains low, affecting approximately 1 in every 5,000 births. While it can seem alarming at first glance, many infants born with gastroshiza can lead healthy lives after receiving proper medical attention and care. Understanding this condition helps demystify its impact on families and healthcare systems alike.
Causes of Gastroshiza
Gastroshiza is a rare congenital condition that occurs during fetal development. The exact causes remain largely unknown, but several factors may contribute.
One theory suggests genetic influences play a role. Certain inherited traits could affect abdominal wall formation, leading to this defect. Environmental triggers might also be significant. Exposure to specific substances during pregnancy—such as drugs or chemicals—could impact the developing fetus.
Maternal health conditions are another area of investigation. Issues like diabetes or obesity have been linked to higher risks for various congenital disabilities, including gastroshiza.
Additionally, nutritional deficiencies in pregnant women may increase the likelihood of this condition. Folate deficiency has long been associated with neural tube defects and could similarly influence abdominal wall integrity.
Further research continues to explore these potential connections, aiming to uncover more about how gastroshiza develops in utero.
Symptoms and Diagnosis
Gastroshiza manifests primarily in newborns. The most noticeable symptom is the external protrusion of abdominal organs, often observed immediately at birth. This condition typically involves the intestines but can also affect other organs.
Parents may notice a bulging mass on the infant’s abdomen. It’s essential to seek medical attention promptly if this occurs. Along with visual signs, gastroshiza can lead to feeding difficulties and potential respiratory issues.
Diagnosis usually happens during pregnancy through ultrasound imaging. Medical professionals look for any abnormal findings that suggest gastrointestinal defects. After birth, healthcare providers conduct physical examinations to confirm the diagnosis.
Additional tests may include X-rays or scans to assess organ placement and function accurately. Early detection plays a crucial role in planning effective treatment options tailored for affected infants.
Treatment Options:
When it comes to treating gastroshiza, there are two primary approaches: surgical repair and non-surgical management. Each method serves different patient needs based on the severity of the condition.
Surgical repair is often necessary for infants. This procedure involves returning the exposed organs into the abdominal cavity and closing any openings in the abdominal wall. Surgeons aim to minimize complications while ensuring proper organ development.
On the other hand, non-surgical management focuses on supportive care. This approach includes monitoring nutritional intake and providing specialized feeding methods. It’s vital for maintaining growth during early stages of life.
Both options require a personalized treatment plan tailored to each patient’s situation, emphasizing collaboration between healthcare providers and families for optimal outcomes.
A. Surgical Repair
Surgical repair is often essential for infants diagnosed with gastroshiza. This congenital condition involves the intestines protruding through a defect in the abdominal wall. Immediate surgical intervention usually takes place shortly after birth.
Surgeons carefully assess the extent of the intestinal exposure and any associated complications, such as damage to the organs or infection. The primary goal is to return the intestines back into the abdominal cavity and close up the defect.
Techniques have evolved significantly over recent years. Minimally invasive approaches are now more common, reducing recovery time and minimizing scarring. Surgeons work closely with neonatologists to ensure that each infant receives comprehensive care during this critical procedure.
Post-surgery monitoring plays a vital role in ensuring successful outcomes. Regular follow-ups help manage any potential complications that may arise, paving the way for healthy development as children grow.
B. Non-Surgical Management
Non-surgical management of gastroshiza focuses on supportive care that can enhance the quality of life for patients. This approach may include nutritional support, vital for infants born with this condition. Feeding strategies often involve specialized formulas or intravenous nutrition until surgical intervention is possible.
In addition to nutrition, careful monitoring and routine assessments are crucial. Healthcare professionals track growth and development closely to ensure the patient thrives despite their condition.
Another aspect involves managing potential complications such as infections or digestive issues. Patients might require medications to alleviate symptoms or prevent further health problems.
Parental education plays a significant role in non-surgical management. Providing caregivers with information about feeding techniques, signs of distress, and when to seek help empowers them in navigating daily challenges effectively. Emphasizing an inclusive support system can significantly ease anxiety surrounding gastroshiza care.
Advancements in Gastroshiza Treatment
Recent advancements in gastroshiza treatment have brought new hope to affected infants and their families. Innovative surgical techniques are now more common, allowing for safer and more effective repairs of the abdominal wall.
Minimally invasive approaches are gaining traction. These methods reduce recovery time and minimize scarring compared to traditional open surgeries. Surgeons can often use smaller incisions while still achieving excellent results.
Technology is also playing an important role. Enhanced imaging tools help doctors assess the condition better before surgery, leading to tailored treatment plans that suit individual needs.
Research into genetic factors has opened avenues for understanding the underlying causes of gastroshiza. This knowledge could pave the way for preventive measures or early interventions in future cases.
As healthcare evolves, so do support systems around gastroshiza care. Parents now have access to comprehensive resources that guide them through every step of managing this complex condition with confidence.
Coping with Gastroshiza: Tips for Patients and Caregivers
Coping with gastroshiza can be a journey filled with challenges, but support is key. For patients, connecting with others who have faced similar experiences can provide comfort and reassurance. Online forums or local support groups are great resources.
Caregivers play a vital role in this process as well. They should prioritize their own well-being to effectively support their loved ones. Taking breaks and practicing self-care ensures they remain resilient.
Establishing open communication within the family fosters understanding and strengthens bonds. Encourage discussions about feelings, fears, and hopes related to gastroshiza.
Routine medical check-ups are essential for monitoring progress. Keep detailed notes of symptoms or changes; this information is invaluable during doctor visits.
Education empowers both patients and caregivers. Understanding the condition helps demystify it, making daily life more manageable. Knowledge promotes confidence when navigating healthcare options together.
Conclusion
Gastroshiza is a complex condition that can be challenging for both patients and their families. Understanding its causes, symptoms, and treatment options is crucial for effective management. Early diagnosis plays a vital role in improving outcomes.
Surgical repair remains the primary treatment method, often yielding positive results when performed timely. However, non-surgical management techniques also offer valuable support for those who may not require immediate surgery.
Recent advancements in technology and medical practices have enhanced treatment possibilities significantly. These innovations provide hope to many affected by gastroshiza, making it easier to navigate this journey with confidence.
For patients and caregivers alike, coping strategies are essential. Seeking support from healthcare professionals can make a substantial difference in managing the emotional toll of this condition.
Living with gastroshiza requires resilience and adaptability but understanding the nuances of this disorder empowers individuals to take charge of their health effectively.